How Well Does Your Body Function?
Runners, hikers, paddlers—we all pick up bad habits after an injury, or when we learn the wrong technique. If that’s you (it probably is), the Functional Movement Screen can point out your weaknesses and get you back on track.
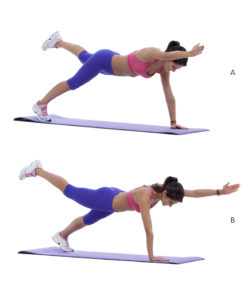
Last month, I found myself in an exercise room, on all fours, straining to hold my body weight while I tried to extend my left arm straight forward and my left leg straight back, then bring my knee and elbow together to touch, all without leaning. (Try it. I dare you. It’s hard.) Corey Vancura, a physical trainer at Timberlane Physical Therapy in Winooski, winced while he watched. He threw me a bone. “Try opposites,” he said.
I put my left leg back on the ground and lifted the right one instead. My insides felt slightly less like they were hanging on by a string. Vancura wrote a note on his chart.
I was in the middle of the Functional Movement Screen, a 20-minute exam that allows the trainer to analyze the test-taker’s functional movements, which put stress on the body’s core muscle groups and systems. Functional movements are movements based on the real-world multi-planar, multi-joint motions that our bodies use on a daily basis.
This particular limb-lifting exercise was called the Rotary Stability Test. A perfect human’s torso would have stayed perfectly stable—no leaning—while that perfect human extended half of his or her limbs and then pulled them back in. That kind of exemplary movement would have earned a perfect score of 3.
I was not a perfect human. But I did complete the test—just with opposite limbs—so I earned a score of 2. All seven movements, which include lunges, leg raises, hurdle steps, push-ups, a shoulder mobility test, and squats, result in a total possible score of 21.
My score? 15. I was one measly point above the threshold for “at risk for injury.” Needless to say, my younger-than-30-year-old body and I were not pleased.
But Vancura made me feel better. “In the three or so years that I’ve been doing the FMS, I’ve never seen a 21,” he said. “When I went to the training course, they said it’s like finding a unicorn.”
I’m not a unicorn. I can live with that. In fact, Vancura most often sees scores ranging between 13 and 15 for athletes in their 30’s. “The score I see most often is 14, which is right at injury risk,” he says.
And the Rotary Stability Test? “I cheat when I do it,” Vancura says. “I go way far out to the side, and I make it look like I can do it so other people think they can do
it. The only person I’ve ever seen do it was my wife. She did it for 20 minutes and was able to get the pattern down.”
It turns out, most adult athletes have developed bad habits—some due to injury, some due to exercising with friends who have bad habits—that have unnaturally altered the way their bodies move. If a runner’s left knee hurts, she might favor her right leg. Or, athletes might be stronger on their right side. “Most people favor their right side, just because the world we live in is right-side dominant,” says Vancura. In fact, only 10 percent of all humans are left-handed, according to a study by Northeastern University, which means most things, like door handles, are designed for right-handed folk.
Incorrect and inefficient movements might feel better in the short term, and it’s even possible to perform well while moving incorrectly.
So, if favoring a non-injured limb doesn’t stop you from running, what’s the problem? What doesn’t tear your ACL only makes it stronger, right? Wrong. The abnormalities and asymmetries of our movements—the caving in of our knees during a squat, or one leg’s inability to stretch as far as the other—can be problematic. We reinforce these poor or inefficient patterns over time, and soon enough, we’re on a fast track to injury.
“Many athletes and individuals are performing high-level activities despite being inefficient in their fundamental movements,” reads a 2014 article titled “Functional Movement Screening: The Use of Fundamental Movements as an Assessment of Function,” published by the International Journal of Sports Physical Therapy.
The article—written by Gray Cook, a licensed physical therapist and orthopedic specialist who founded the Functional Movement Screen*, and three others—makes a case for the use of FMS in preseason sports testing. Gray and the authors argue that physical therapists too-often neglect the body’s bigger picture, and that the FMS can help prevent injury.
Plus, it’s difficult to improve performance when our biomechanical movements—interactions between our muscles, ligaments, bones and joints—aren’t up to snuff. While the FMS does not claim to improve performance—only to predict and prevent injury—the authors state: “The best equipment and programs cannot improve fitness and health if fundamental weaknesses are not exposed.” To become a self-aware athlete, you need a good picture of your entire body.
What Is The FMS?
Simply defined, the FMS is a multi-part screen that allows trained professionals to assess the fundamental movements of athletes, and then predict whether those athletes are at risk for injury. The screen is standardized—trainers can only become certified after enrolling in several-day-long workshops.
It uses the kinetic link model, which depicts the body as a system of linked, interdependent segments. While independent tests by clinicians might focus on a singular muscle or group of muscles, the FMS focuses on movement patterns.
During the screen, the trainer places the athlete in seven “extreme” positions, like squats and lunges, to analyze how the body’s muscles and joints work together. They watch closely for imbalances, weaknesses and asymmetry, and rate the athlete on a scale from 0 to 3.
Zero means the athlete felt pain during a movement, one means the athlete could not complete the movement, two means the athlete could complete the movement with some modification, and three is a perfect score.
The screen’s structure means that the FMS can identify weaknesses that other fitness tests can’t. Take this example from the IJSPT’s 2014 article:
“(A person may have) an above average score on the number of sit-ups performed during a test, but is performing very inefficiently by compensating and initiating the movement with the upper body and cervical spine (neck) as compared to the trunk. Compare this person to an individual who scores above average on the number of sit-ups, but is performing very efficiently and does not utilize compensatory movements to achieve the sit-up. These two individuals would each be deemed ‘above average’ without noting their individual movement differences.”
The objective of the FMS is to categorize these two movements as different—and ultimately, to help the under-performing athlete gain self-awareness and understand how to correct weaknesses.
The screen was designed by Gray Cook in 1997 in Danville, Virginia. He started to screen kids in public high schools near his clinic, and realized that many of them had chronic pain. So, with fellow physical therapist Lee Burton, he started trying determine the source of the pain with a series of tests. Out of that emerged a pre-participation physical they used on hundreds of athletes.
“Gray had a very unique way of evaluating people—how to look at the parts of the body, and not just how to look at how the parts worked, but how the parts affected areas,” Burton says. “He was looking at movement patterns during his evaluation of something as simple as an ankle sprain.”
For the first several years, Gray and Burton presented the information everywhere they could—at conferences and lectures all around the country. Soon, FMS was picked up by Division I universities, professional teams and hospitals. Now, the National Football League, National Hockey League, Major League Baseball and several European soccer teams use it during pre-season.
The first study conducted with the FMS, called “Can Serious Injury in Professional Football be Predicted by a Preseason Functional Movement Screen?” was not published until 10 years after the screen was developed, in 2007. The answer was ‘yes’—it found that professional football players who had dysfunctional fundamental movement patterns (which were measured using the FMS before the season started) were more likely to suffer an injury than those with a high score.
Not only do athletes come away from the screen with a better understanding of their weaknesses, they also learn how to improve. When the screen is complete, the results are entered in a system called “Move 2 Perform,” which provides three simple exercises tailored for the athlete’s weaknesses. The program also provides a detailed run-down of how you did on each test, and churns up statistics like how you compare against other people in your age group.
Vancura told me my weakest areas were core and hip strength, so I walked away from Timberlane with a regimen of shoulder taps (plank position, touch one hand to the opposite shoulder, count to three, then switch); quadrupled diagonals (all fours, extend the left arm and right leg, hold for 5, then switch); and the push up walk out (a forward bend walked out to a plank—hold, and walk it back).
Often, the physical therapist or clinician who administers the screen can schedule sessions to work on weaknesses, too. At Timberlane, the screen is free. (See “Where to Get Screened” for other member clinicians in Vermont.)
Who Should Take The FMS?
For most athletes, getting screened is a good idea. The FMS can identify deficits in the movements involved in most sports, and can promote self-awareness for all athletes.
But the trainer can pay extra-close attention to the movements that are particularly important to your sport. For example, one of the seven moves, called the hurdle step, gives a good picture of what a runner might look like in action. It requires athletes to step over a line suspended between two wooden posts at the height of their knee.
“That’s the height where you should be able to pick your foot up in a dead-out sprint,” Vancura says. “If you can’t do that, and you have to be moving over to the side to put your leg over, that means you don’t have enough hip strength in that one leg.”
The in-line lunge simulates stress during rotational, decelerating and lateral movements, along with hip and ankle mobility and stability. It requires the athlete to balance on a balance-beam type support, so as to resist rotating. That one helps Vancura identify problems that hikers might have.
“That mimics walking up the hill and stepping onto a rock as you push yourself up,” he says. “If you don’t have that balance on that other leg, you’re more likely to fall. Or, you could rely on trekking poles and overuse your shoulders, rather than actually using your hip and finding other ways to get yourself up the hill.”
Vancura says weekend warriors are particularly good candidates for the FMS. “They might be at a desk job Monday through Friday, and then Saturday and Sunday they want to ski, or they want to snowshoe, they want to run or bike,” he says. “They want to stay active, but they don’t know how to integrate exercises in their work day without having to go to the gym.”
In other words, the less consistent the training regimen, the more likely that athlete is to become injured. All the more reason to get out there every day—with some self-awareness about functional movement.
Eds. note: Gray Cook and Lee Burton, two of the four authors of the two-part article titled “Functional Movement Screening: The Use of Fundamental Movements As An Assessment Of Function,” published in the International Journal of Sports Physical Therapy, are associated with functionalmovement.com and profit from the sale of functional movement products. A note within the article reads: “The Editors of IJSPT emphasize (and the authors concur) that the use of fundamental movement screening as an assessment of function is the important concept to be taken from Part I and Part II of this series and such screening can be performed without the use of any trademarked equipment.”
Where to Get Tested:
Fit 2 Function VT
Bennington, VT
Trainer: Julie Horst
(802) 384-3423
Green Mountain Orthotic Lab
Bondville, VT
Trainer: Bill Haight
(802) 875-1122
Move Fitness
Waitsfield and Randolph, VT
Trainer: Sarah Larmie
(802) 558-8481
Parisi Speed School
Williston, VT
Trainers: Casey Lee and Joe Grunwald
(802) 488-3278
Timberlane Physical Therapy
Winooski, VT
Trainer: Corey Vancura
(802) 864-3785

