Vermont Is Counting Ticks… And Tracking Lyme Disease
[Updated on July 30, 2019]
Preliminary spring data is in from the Vermont Agency of Agriculture, Food & Markets (VAAFM) and Vermont Department of Health’s systematic tick surveillance program. A total of 1,924 ticks were collected in the 2019 spring sampling.
“Tickborne diseases are on the rise in Vermont,” said Governor Phil Scott. “Any time a tickborne illness appears in a community, it’s a cause for concern. The good news is we can still enjoy outdoor activities by knowing how to protect ourselves from tick bites.”
The systematic tick surveillance program was initiated in 2018 by the Health Department in partnership with VAAFM to track blacklegged ticks and the pathogens they carry around the state. In 2018, a total of 1,239 ticks were collected during the spring, although due to a change in the way ticks are collected, data from 2018 can’t be compared to this year’s figures.
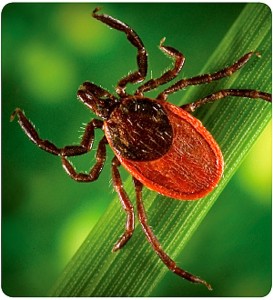
The program focuses on the blacklegged tick, which is responsible for transmitting over 99% of all tickborne diseases reported in Vermont. Through this program, ticks are collected in the spring and fall from locations around the state. Once all data has been collected, VAAFM and the Health Department collaborate to calculate blacklegged tick densities, in order to determine the likelihood of human encounters with ticks that can transmit disease.
After each collection period, ticks are sent to the Centers for Disease Control and Prevention (CDC) for identification and testing of blacklegged ticks for five tickborne pathogens: Borrelia burgdorferi (the pathogen that causes Lyme disease), Anaplasma phagocytophilum, Babesia microti, Borrelia miyamotoi, and Powassan virus. Pathology results from the CDC for 2019 are pending.
How We Started Counting Ticks
Wildlife biologist Alan Giese has spent much of his time studying peregrine falcons, bald eagles and even California condors. But as the days warmed up in the spring of 2016, the Lyndon State College professor and his biology students were bashing through the fields and forests of Vermont doing what most of the rest of us try to avoid doing: collecting ticks.
That spring, Giese set up 12 monitoring stations around the state where he can collect ticks and then dissect them to determine if they carry the Lyme disease bacteria, Borrelia burgdorferi. Since 2013, he’s captured and tested more than 800 ticks.
In the last several years, he’s sent them on to the University of Vermont’s Dr. Ralph Budd, Director of the Vermont Center for Immunology & Infectious Diseases. In an effort to determine what strains of Lyme disease ticks are carrying and how it is spreading, Dr. Budd and his team have become the first to sequence the DNA in the gut of ticks.
What both Dr. Giese and Dr. Budd, and, in fact scientists around the Northeast, are trying to figure out is why Vermont has become the second most prevalent place in the country for incidence of Lyme disease, per capita, after Maine.
“When I moved to Vermont 20 years ago, about 10 percent of the ticks in the state were infected with Lyme disease,” says Dr. Budd. “Today, it’s about 50 percent.”
The rise in the numbers of humans who have contracted Lyme disease has increased accordingly. In 2005, only 54 cases were reported, according to the Centers for Disease Control. By 2013, that number had risen to 674, before dropping to 442 in 2014 (the last year on record). “What we are seeing is that the tick population is moving north,” says Dr. Budd. “Right now, the highest incidence is in southern Vermont.”
The Carriers
Lyme disease was first reported in Lyme, Connecticut in 1975. At the time, it was mistaken for arthritis. Early symptoms are often just like the flu: fever, aches and muscle soreness but can progress to include weakness in the legs and arms, facial paralysis and problems with short term memory. It wasn’t until 1988 that it was reported in Vermont.
One of the things Dr. Budd has been on the lookout is how Lyme disease travels. Though the deer tick, or black-legged tick as it is also called, is the primary carrier of Lyme disease, Dr. Budd pointed out that it’s primarily field mice that are transporting it. “Dogs, cats and even cows can get Lyme disease too,” he warns. For that reason, the highest incidences of infected ticks are found in fields and around farms.
“There’s no doubt that as we see climate change continue to happen, that Lyme disease will continue to move north,” he says. “And as much as Borellia migrates, it will mutate, just like the flu mutates.” for is new mutations of Lyme, as well as other diseases.
Already two other tick-borne diseases are showing up in Vermont, babesiosis and anaplasmosis, both with similar, but more severe symptoms. More than 115 cases of anaplasmosis have been confirmed around the state, but primarily near Rutland and Bennington counties and a third of those required hospitalization.
Unlike Lyme disease, babesiosis and anaplasmosis don’t show up with a bull’s eye. But, as Dr. Budd notes, Lyme disease doesn’t always either.
Another disease, called Powassan, is making headlines. Scientists have estimated that only one percent of ticks in Vermont carry the disease, but it’s incurable, and can be deadly, causing inflammation of the brain. Symptoms include headache, fever, vomiting, seizure, speech difficulties, weakness and confusion. While Lyme disease is transmitted over a period of 24 hours, a tick can infect a human with Powassan minutes after the first initial bite.
“It’s not always an easy bug to diagnose—only one in three people ever get the tell-tale ‘bull’s-eye’ rash that’s associated with an infected tick bite,” admits Dr. Budd. “But the good news is, it is treatable.” For most a course of two weeks of antibiotics two times a day will knock out the disease. “The problem we are seeing,” says Dr. Budd, “is after the bug has been killed our bodies are still worn down. People continue to have symptoms but when they get tested, they are told they no longer have the disease. No one is denying that the symptoms aren’t real but using more long-term antibiotics is like throwing water on a house that’s already burned to the ground—it’s not going to fix the house.”
Instead, Dr. Budd looks to arthritis medications. “Your immune system is so used to fighting the disease that it doesn’t stop and that’s what causes the inflammation and arthritis. Most of the time we see using medicines that treat arthritis will work on these lingering symptoms.”
The best approach is to avoid getting bitten in the first by wearing long pants and sleeves. May, June and July are the worst seasons and ticks often congregate in high grass areas and where there’s lots of leafy debris.
Once home, shower as soon as you can and wash your clothes in hot water and dry them at high heat, to kill any ticks.
If you do find a tick on you, get it off with fine-tipped tweezers. It can take a tick up to 36 hours to transmit the disease so the sooner you can get it off the better.
If you do have Lyme disease, it may take up to two weeks for symptoms to show.

