Haglund’s Heel and Achilles Tendonitis
By
Robert Rinaldi, DPM
Posted March 6th, 2009
Most everyone has heard of the mythical Greek athlete and warrior, Achilles, and his problem heel, but not many know about the bane of the running athlete: Haglund’s Heel. Dr. Haglund was a friend of Dr. Roentgen, the inventor of the x-ray. Haglund began researching the boney anatomy of humans for his dear friend, and came up with a fairly common deviation of the calcaneous, which became known as Haglund’s Heel. I am pretty sure that Haglund never guessed that his discovery would be associated with Achilles tendonitis and athletic disability.
CALCANEAL DEFORMITY
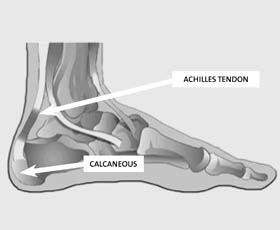
Haglund noted that there are times when the most posterior/superior aspect of the heel bone forms into a “beak.” This beaking can put undo pressure on the structures behind it, especially the Achilles tendon, which attaches to the calcaneous about midline along the posterior vertical wall of the bone. The soft fibers of tendon are separated and cushioned from the hard boney substances by a bursa, known as the retero-calcaneal bursa. The “beaking” that bears Dr. Haglund’s name is a deformity that can put increased pressure on the bursa, causing it to inflame. In turn, this will create restriction on the function of the Achilles tendon, causing injury to its vertical fibers.
HYPERPRONATION
Often, biomechanics of the foot plays a very important role in the mechanism and production of foot injuries. Pronation is a normal motion and is the primary shock absorber within the foot. During the gait, when a typical foot approaches the ground, the forefoot tilts inward. Just before heel strikes ground, the foot’s sole faces inward on a slight angle. This position is known as forefoot varus. As your foot continues to make contact, the varus position alters until the foot is in full contact with the horizontal surface beneath it. When the forefoot varus tilt is too great, the foot must travel excessively. This excess motion is called hyperpronation.
HOW DOES HYPERPRONATION CAUSE ACHILLES INJURY
When a foot hyperpronates, the forefoot travels an increased distance and the rear part of the foot follows. The posterior surface of the calcaneous will move and finish its motion slightly tilted inward. A shearing force is created against the retero-calcaneal bursa and also against the Achilles tendon. When Haglund’s deformity is concurrently present, pressures are ramped up in each gait cycle. When this complex set of circumstances is associated within the runner, the factors are multiplied greatly by gravitational forces. The pounding and shearing action against the bursa and the Achilles tendon will cause inflammation, stiffness, pain, and dysfunction.
TREATMENT PLANS
A conservative approach is to insert heel lifts in the running shoes. They will change the angle of the posterior aspect of the calcaneous. A quarter-inch resilient heel lift is best. Spenco makes my favorite, and they are inexpensive, durable, and easy to find in most running stores. Often they will solve the problem. Try them if you are suffering from posterior heel pain and morning Achilles stiffness. The result should be almost miraculous.
If heel lifts don’t work, you should schedule a visit to a sports medicine provider. X-rays are important and should be taken at the outset of your exam. Your biomechanics should be evaluated. If hyperpronation is present, it should be controlled with a combination of athletic shoes and orthotics. My personal favorite shoe for control of mild hyperpronation is still the Asics GT 2140, but now I have added the Saucony Progrid Guide to my list, which has become a favorite of women runners.
I have been using intrinsically posted polypropylene orthotics for more than 30 years. They require no so-called “break-in,” and take no room in the shoe, so size and fit are not altered. They will never wear out, and I mean never! A regimen of non-steroidal anti-inflammatory drugs is routine in my treatment plan. Steroid drugs are contra-indicated for Achilles injuries, so please refuse any attempt or suggestion that they be used. More than 85 percent of the time, patients will respond to conservative treatments, but if failure continues, surgery becomes the treatment of choice.
SURGICAL RESHAPING OF THE CALCANEOUS
When all else fails, including altering your exercise and workout routines, surgery becomes the option. The procedure involves reshaping the posterior, superior portion of the heel bone. This is often called a Haglund’s Repair. Post-operatively, the procedure will necessitate using a cast or cam-walker for several weeks. The risk of surgery includes injury and even rupture of the Achilles tendon. The surgical procedure is performed in an area that sits just in front of the Achilles tendon, and there are times that a portion of the Achilles must be detached from the calcaneous. These factors increase the risks for complication. Under most circumstances the procedure and post-op course proceed without incident, and the athlete is able to return to all activities free from pain. Overall, surgical outcomes are excellent.
Robert Rinaldi is a board-certified podiatrist and podiatric surgeon at the Gifford Medical Center in Randolph, VT. He is a fellow and a founding member of the American Academy of Podiatric Sports Medicine, and a podiatric consultant to the Dartmouth College track and cross-country teams. He is a former nationally ranked long-distance runner, having competed in 25 world-class marathons.
You can reach him at Gifford Sports Medicine and Surgery Clinics in Randolph, VT, or at the Sharon Health Clinic in Sharon, VT, 802-728-2490 or 802-763-8000 or at rrinaldi@giffordmed.org.
